314
Views & Citations10
Likes & Shares
Conclusion: Dengue hemorrhagic fever during pregnancy requires a multidisciplinary approach. Timely intervention and aggressive management are the key to its positive outcome. Uterine artery embolization is a lifesaving procedure in the patients where there is bleeding due to thrombocytopenia or dengue hemorrhagic fever.
Keywords: Thrombocytopenia, Postpartum hemorrhage, Uterine artery embolization
CASE REPORT
23-year-old primigravida was referred from periphery with dengue NS1antigen positive and platelet count of 49000. She had complaints of fever with nausea and vomiting and epigastric pain for 3 days. At the time of admission, she was febrile (102°F), pulse rate was 114 per minute and blood pressure was 92/60mmHg. On abdominal examination - Uterus was term size, single live fetus with cephalic presentation. Non-stress test (NST) was normal. On per vaginal examination cervical so was closed (Tables 1 & 2).
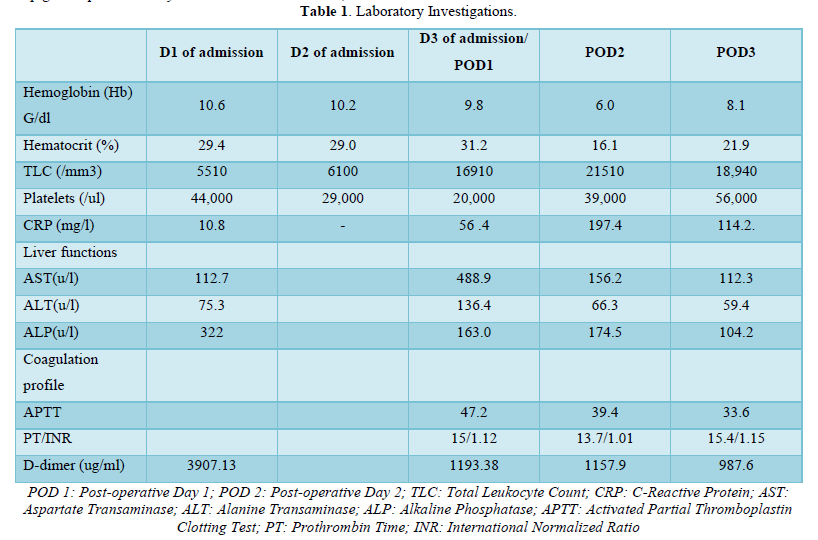
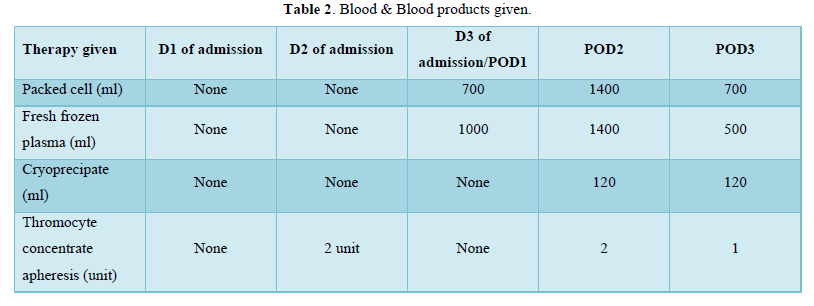
Laboratory investigations showed hemoglobin 10gm/dl, platelets 44000, elevated liver enzymes, B negative blood group. A diagnosis of full-term pregnancy with dengue with warning signs was made. The patient was admitted in Medical ICU. On Day 2 of admission her platelets dropped to 29000 for which 2 units of Thrombocyte concentrate were transfused. NST was reactive and woman had no fresh complaints. On Day 3 of admission, fetal distress developed as was diagnosed on NST. Her Platelet count was 29000, Coagulation Profile was normal with International Normalized Ratio (INR) 1.1 and other reports were normal. With high-risk consent of hemorrhage and with arrangement of 4U Packed Red Blood Cell (PRBC) and 8 U FFP, woman was taken for Emergency LSCS under General Anesthesia. A live male child weighing 2.8 kg was delivered and was shifted to Neonatal Intensive Care Unit (NICU). There was mild to moderate Postpartum Hemorrhage (PPH) intraoperatively which was managed by 600mcg of misoprostol, 20 units of oxytocin, Methergine 100mcg intramuscular. As her blood group was B negative, there was non-availability of Platelets of the same blood group. Thus, she was transfused 2 Units of PRBC and 6 Units of FFP intraoperatively. A subcutaneous drain was kept as there was oozing from the subcutaneous tissues and woman shifted to ICU for observation. 8 h after Cesarean section there was bleeding from stitch line and drain site. Her hemoglobin dropped to 6 g/dl, Total Leukocyte Count (TLC)-21510, platelets-29000, C-Reactive Protein (CRP)-197.0, procalcitonin-65, activated Partial Thromboplastin Clotting Time (APTT)-47.2, INR-1.12. Woman was actively and aggressively managed with multi-disciplinary approach. She was transfused 6 Units (120ml) of cryoprecipitate, 6 Units (1200ml) of FFP, 4 Units (1400 ml) of PRBC, 2 units of thrombocyte concentrate (Single Donor Platelets) over the period of 12 h. On postoperative Day 2, her abdomen was found to be distended and tender. Possibility of intra-abdominal bleeding was suspected. Laboratory investigations showed hemoglobin 8.1g/dl, TLC 18940, platelets 56000, CRP- 114, INR- 1.01. There was ascites, pedal edema. X-ray chest showed bilateral pleural effusion. 2D echo was normal. Urinary output was maintained. Diuretics were given to treat fluid overload. Extensive supportive treatment was given along with higher broad spectrum antibiotic Meropenem. Bilateral venous doppler of lower limbs was done on complaints of pain in left lower limb but there was no evidence of deep venous thrombosis. Along with the opinion of intervention radiologist, Uterine artery embolization was decided as the further management to stop intra-abdominal bleeding. Selective cannulization of each uterine artery was done with micro catheter. Distal embolization was done by gel foam thus preserving the fertility of woman. Proximal embolization of bilateral uterine artery was done by coils. Post embolization woman was transfused with 2 Units (700ml) of PRBC and 2 Units (500ml) of FFP. Gradually the bleeding from stitch line and drain site stopped. The vitals of the woman gradually improved. She was transferred from Medical ICU to high dependency unit (HDU) and then to postnatal ward. During recovery phase she was afebrile and vital parameters remained stable. Laboratory investigations showed hemoglobin 10.3g/dl, WBC count 10840, platelets count 1.86 lakhs/cumm. Antibiotics were continued for 7 days. Subcuticular drain was removed on 7th postoperative day. Anti- D was given within 72 h of delivery. Woman and her baby were discharged on post-operative Day 11.
DISCUSSION
Dengue hemorrhagic fever in pregnancy requires a high index of suspicion and quick management. Dengue fever presents in 3 phases [1].
Acute febrile phase: with high grade fever with nausea and vomiting with sore throat. Rash may and may not be present. Tourniquet test is positive.
Critical phase: when the fever subsides, the phase of capillary leak occurs due to which hemorrhagic complication develops and, in this phase, multiple organ involvement happens. There is progressive fall in White Blood Cell (WBC) count, low platelets count, rise in Packed Cell Volume (PCV) / Hematocrit. Signs of shock may appear.
Recovery phase: as the patient survives the critical phase gradually the extracellular fluid reabsorption takes place. The patient becomes hemodynamically stable, WBC rises, platelets rises and PCV reduces due to fluid reabsorption. Complications in this phase are rare. Pulmonary edema and hypervolemia may occur at this time due to excessive fluid overload. In the event of thrombocytopenia during the critical phase, severe bleeding can complicate the delivery. Induction of Laboure or caesarean section should be avoided during the critical phase. If delivery is inevitable blood and blood products should be properly cross matched and saved. If platelet count is less than 50,000/ul, platelet transfusion should be done before delivery [8]. Atony of uterus should be avoided by timely use of uterotonics. In our case general anesthesia was given due to thrombocytopenia present [9]. Regional anesthesia can also be considered if the platelets count is above 70,000/ul. In our case although prophylactic transfusion was done but bleeding was observed due to defect in hemostatic system secondary to dengue infection. The complications of infection depend on the interaction of virus with the host. The virus multiples in the cells and causes an antigen antibody reaction [10]. Thrombocytopenia results from immune mediated destruction of platelets [11]. However, it co-relates poorly with bleeding manifestations as seen in our case. It can be used as a prognostic indicator rather than as a parameter for therapeutic interventions [12]. Plasma leakage and intrinsic coagulopathy are the fundamental pathological changes responsible for the morbidity and mortality associated with dengue hemorrhagic fever [13]. In our case in spite of transfusion of blood products and fresh frozen plasma there was life threatening intra-abdominal bleeding which did not subside on conservative treatment. Uterine artery embolization is a possible intervention which can be considered in such cases. Uterine artery embolization was successfully carried out by using gel foam of about 4mm in diameter in size in our case. Generally, it takes about 5/6 weeks for the vessels to recanalize and the blood flow returns to normal [14].
Pregnancies after UAE can have higher rates of miscarriage, and are more likely to have a cesarean section and postpartum hemorrhage. Though such complications are mentioned after the UAE but here it was a lifesaving procedure and thus must be considered in such cases.
- World health organization (2009) Dengue guidelines for diagnosis, treatment, prevention and control: new edition; World Health Organization. Geneva. Switzerland pp: 147.
- Dengue in Pregnancy (2015) Management protocol fogsi. Available online at: https://www.fogsi.org-2015/11
- Sharma S, Jain S, Rajaram S (2016) Spectrum of maternal fetal outcomes during dengue infection in pregnancy: An insight. Infect Dis Obstet Gynecol 16: 1-4.
- Sellahewa KH (2013) Pathogenesis of dengue hemorrhagic fever and its impact on case management. Int Sch Res Notices 2013: 571646.
- Rathore SS, Oberoi S, Hilliard J, Raja R, Yogesh V, et al. (2022). Maternal and fetal-neonatal outcomes of dengue virus infection during pregnancy-Systematic Review. Trop Med Int Health 27(7): 619-629.
- Gonsalves M, Belli A (2010) The role of interventional radiology in obstetric hemorrhage. Cardiovasc Intervent Radiol 33: 887-895.
- Phupong V (2001) Dengue fever in pregnancy: A case report. BMC Pregnancy Childbirth 1: 7.
- Friedman EE, Dallah F, Harville EW, Myers L, Breart G, et al. (2014) Symptomatic dengue infection during pregnancy and infant outcomes: A retrospective cohort study. PLos Negl Trop Dis 8(10): e3226.
- Witaya TP (2003) Parturient and perinatal dengue hemorrhagic fever. Southeast Asian J Trop Med Public Health 34(4): 797-799.
- Martina BEE, Koraka P, Osterhaus ADME (2009) Dengue virus pathogenesis: An integrated view. Clin Microbiol Rev 22(4): 564-581.
- Sellahewa KH (2013) Pathogenesis of dengue hemorrhagic fever and its impact on case management. Hindawi. Available online at: http://dx.doi.org/10.5402/2013/571646
- Wills B, Tran VN, Nguyen TH, Truong TT, Farrar J, et al. (2009) Hemostatic changes in Vietnamese children with mild dengue correlate with the severity of vascular leakage rather than bleeding. Am J Trop Med Hyg 81(4): 638-644.
- Kaufman RM, Gary KS, Aryeh S, Babu GW, Edward CW, et al. (2015) Platelets transfusion: A clinical guideline from the AABB. Ann Intern Med 162(3): 205-213.
- Ooi ET, Ganesananthan S, Anil R, Kwok FY, Sinniah M (2008) Gastrointestinal manifestations of dengue infection in adults. Med J Malaysia 63(5): 401-405.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Microbiology and Microbial Infections (ISSN: 2689-7660)
- Proteomics and Bioinformatics (ISSN:2641-7561)
- Food and Nutrition-Current Research (ISSN:2638-1095)
- Journal of Veterinary and Marine Sciences (ISSN: 2689-7830)
- Journal of Biochemistry and Molecular Medicine (ISSN:2641-6948)
- Journal of Genomic Medicine and Pharmacogenomics (ISSN:2474-4670)
- Journal of Agriculture and Forest Meteorology Research (ISSN:2642-0449)

